LYMPHEDEMA
Author: Dr Adrian Ooi
Lymphedema is a condition characterized by swelling in the extremities (arms and/or legs). The lymphatic system is responsible for the part of the immune system and the return of waste, excess fluid, and fat to the central circulation. The swelling occurs when lymph nodes or channels are no longer facilitating the proper drainage of lymph fluid from an area of the body. Lymphedema features can range from mild, intermittent swelling, to persistent swelling with gross skin changes.
Causes of Lymphedema
Lymphedema causes can be primary, due to a congenital condition, or secondary, which is caused by infection, trauma or, most commonly in the developed world, treatment of cancer. Lymphedema affects some cancer survivors who have been treated for breast cancer, gynecologic cancers, melanomas and other types of skin and urologic cancers. This occurs because the normal lymphatic flow of the peripheries has been affected by cancer treatment. The onset of symptoms may be delayed by months or even years after the initial injury.
Clinical features of Lymphedema
Lymphedema symptoms typically worsen over time. In the early stages, there can be mild swelling which is reversible. Eventually, the swelling may become irreversible and skin changes may occur. In the extreme form of lymphedema, elephantiasis can occur. Features to look out for:
- Clinical features of lymphedema
- Excess fat or fluid in the extremity
- Change in skin quality such as skin fibrosis
- Extremity tenderness or pain
- Cellulitis
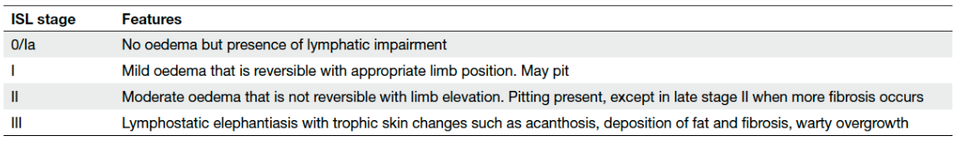
The International Society of Lymphangology (ISL) classifies lymphedema according to the following stages:
Assessment of Lymphedema
Your plastic surgeon will ask you a range of questions to determine the severity of your lymphedema, and decide on the optimal treatment modality. Part of the assessment may involve limb measurements and medical photography. If required, you may be asked to undergo investigations such as lymphoscintigraphy, indocyanine green lymphangiography, and/or MRI.
In many cases, an excess of fatty tissue, a condition called LIPEDEMA, may be concurrently present, or be the main cause of the limb swelling.
TREATMENT
Lymphedema treatment can be divided into conservative or surgical measures. Medical measures are limited to the treatment of symptoms such as antibiotics for infection. The decision about which type of treatment you receive should be based on a discussion between you and your plastic surgeon. Treatment plans are individualized for each patient based on the clinical stage of lymphedema and anatomical considerations. Before undergoing treatment, you should discuss your expectations with your surgeon, and maintain a positive outlook while keeping with realistic goals through the process.
Conservative Treatment
Conservative management is carried out with the help of a lymphedema therapist. These therapists are specially trained to assess and follow-up for your lymphedema. Therapy may include moisturizing of skin, manual lymphatic drainage, lymphatic massage, physiotherapy and compression therapy. The latter may be life-long, regardless of whether surgery is performed. In many instances, weight loss helps with reducing the severity of lymphedema as well.
Surgical Treatment
Surgery for lymphedema is most often performed in a hospital setting, possibly including a short hospital stay. Depending on the type of surgery, it can be done under local or general anesthesia.
Surgical treatment of lymphedema can be further subdivided into excisional and physiological techniques. Excisional procedures aim to remove excess skin and soft tissue to decrease bulk and facilitate hygiene. These operations are usually recommended for patients with advanced-stage lymphedema with significant skin changes. Liposuction has also been used to treat patients with advanced lymphedema with mainly excess fat.
Physiological surgical treatment options include Lymphatic Bypass Procedures, where lymphatic vessels are connected and drained into the body's venous system and Vascularized Lymph Node Transfer, where lymph nodes are harvested from one part of the body and surgically implanted in the affected area to rebuild a failed system. Women who are seeking both breast reconstruction and treatment of arm lymphedema may be candidates for autologous breast reconstruction with attached lymph nodes.
After Your Procedure
You will usually be hospitalized for a few days after your procedure. In excisional procedures, this is done to monitor for bleeding, infection and pain. In physiological procedures, bleeding and pain are less likely, but your lymph node transplant does require monitoring. There will be bandages and possibly wrapping and drains at the post-operative site.
You are usually able to walk on the first day after the procedure. The physical and lymphedema therapists will help you with this as well as compression, which still has to continue post-operatively. You can return to light exercise at about 3-4 weeks after the procedure, and full activity at about 6 weeks post-operatively. If the lymphedema improves, patients may gradually decrease their dependence on nonsurgical strategies. However, if it worsens, additional surgical interventions can be considered.
Although lymphedema surgery almost always improves the physical and psychological (qualitative) symptoms of lymphedema, the quantitative results are variable. Your plastic surgeon and therapist will follow you up closely after the procedure. Please follow the post-operative instructions and attend follow-up visits as scheduled.
COMPLICATIONS AND MANAGEMENT
Your plastic surgeon should explain in detail the risks associated with lymphedema surgery. These risks depend on the type of procedure performed. The general risks include, but are not limited to, bleeding, infection, fluid collection, poor healing of incisions and anesthesia risks. Incision lines for surgery will be visible, including at potential donor sites in the neck, abdomen or groin region. For the vascularized lymph node transfer, there is the risk of partial or complete loss of the flap and a loss of sensation at both the donor and reconstruction site. A very rare complication of vascularized lymph node transfer is donor site lymphedema caused by damage to the donor site lymph nodes. However, with proper surgical technique and imaging, this risk is minimal.
