BREAST RECONSTRUCTION
TYPES OF RECONSTRUCTION
Author: Dr Chia Hui Ling
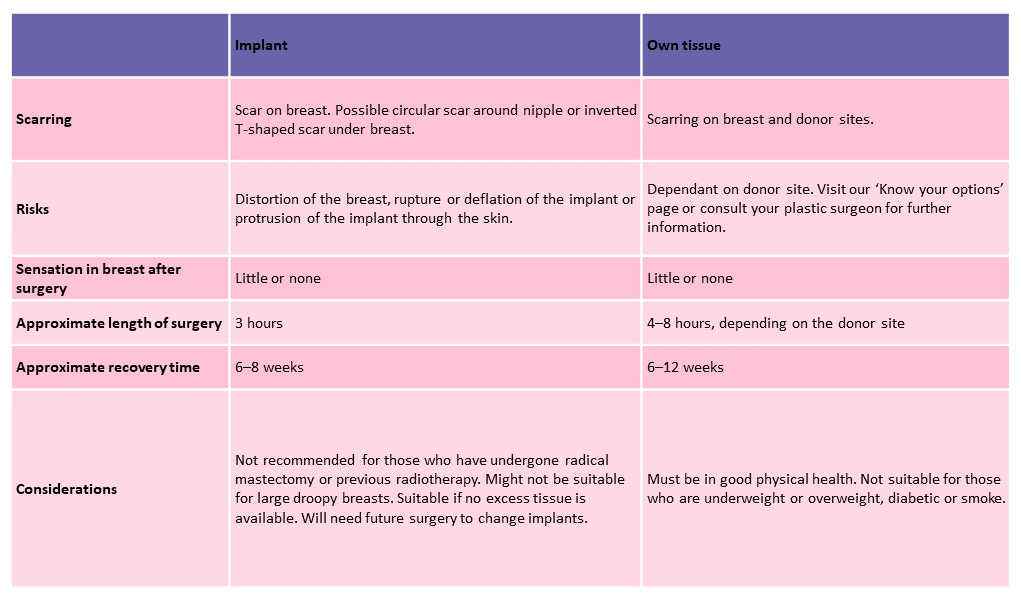
Difference between implant and own tissue breast reconstruction
Own Tissue Reconstruction
Own tissue reconstruction involves the use of your body’s own tissues in the reconstruction of your breast. By using your own living tissue, your breast will not only look and feel more natural but will also change as your body changes, literally growing and ageing with you. There are four types of tissue that can be used:
Abdominal Flap
The lower abdomen is the most common site for retrieving the tissue needed to reconstruct the breast. There are many names for the abdominal surgery used for reconstruction, including TRAM, DIEP and SIEA, depending on the source or pattern of blood supply to the abdominal skin and fat.
What are the common complications of TRAM flap reconstruction?
What can i expect after surgery?
After surgery, you will be nursed in a ‘bending’ position. Tubes will be inserted into your wounds to drain excessive fluids from surgical sites. In addition, you may experience tightness in your abdomen, which should subside in 2-3 weeks.
Your total hospital stay can be between 4-10 days and you would be expected to be out of bed and mobile 1-2 days after the surgery. Upon discharge, you may still have one or two tubes in your wounds to drain any excess fluids, but these will be removed at follow-up appointments at the out-patient clinic.
Thigh Flap
Extra skin and fat known as Transverse Myocutaneous Gracilis (TMG) or Transverse Upper Gracilis (TUG) flap from the inner thigh can also be used for breast reconstruction.
In this procedure, the gracilis muscle in the inner thigh and its blood vessels are removed together with its overlying skin and fat, disconnected and transferred into the breast pocket to reconstruct the breast.
The blood supply to the gracilis muscle and the overlying skin is then reconnected to keep it alive. This requires microsurgery expertise. Usually, blood vessels in the chest are used.
Gluteal flap
In gluteal flap breast reconstruction, the gluteal flap, which consists of skin and fat from the buttock, is transferred to the breast. There are two types of gluteal flaps: the SGAP flap, in which the upper buttock skin and fat is used, and the IGAP flap, where the skin and fat of the lower buttock is used. Once the tissue has been transferred, microsurgical techniques are used to re-establish the blood flow into the flap.
Back Flap
The back flap or latissimus dorsi (LD) is a broad muscle in your back. In this procedure, the LD muscle, along with its overlying skin and fat, is transferred to the front of the chest for breast reconstruction.
But with improved surgical techniques, it is now possible to take only skin and fat tissue from the back. Located in the same region as the LD flap, the thoracodorsal artery perforator (TAP) flap is a small flap that can be used for reconstructing small/partial breast defects, such as in lumpectomy patients. This flap preserves the LD muscle and consists of only skin and fat.
Implant Reconstruction
Implant breast reconstruction uses breast implants to restore the shape and volume of the breast. There are two main types of implants available: silicon and saline. Depending on the condition of the breast after mastectomy, implant breast reconstruction may be done in one or two stages.
Implants, however, may not be suitable for every woman, particularly those who have undergone radical mastectomy (with removal of chest muscle) or previous radiotherapy. Talk to your surgeon about the options available to you.
Oncoplastic Breast Surgery
Oncoplastic surgery involves the use of plastic surgery techniques to reshape the remaining breast or reconstruct the breast after breast cancer surgery. It corrects the imbalance between the unaffected and affected breast after removal of the tumour and prevents undue scarring and deformation of the breast for an aesthetically pleasing outcome.
There are two types of oncoplastic techniques: volume replacement and mammoplasty volume displacement.
